Advances in Parkinson’s Disease Research & Treatment Options are revolutionizing our understanding and management of this debilitating neurological disorder. Recent breakthroughs in understanding disease mechanisms, coupled with the development of novel therapeutic strategies, offer renewed hope for patients and their families. This exploration delves into the latest research, examining current and emerging treatments, diagnostic advancements, and lifestyle factors influencing disease progression. We will explore the complexities of Parkinson’s, from its underlying causes to the promising avenues of future research.
The journey to effectively combat Parkinson’s disease involves a multifaceted approach. This includes unraveling the intricate interplay of genetic predispositions, environmental triggers, and the progressive neurodegeneration characteristic of the illness. We’ll examine the efficacy of existing treatments, such as levodopa and deep brain stimulation, while also exploring the exciting potential of emerging therapies like gene therapy and immunotherapy. Understanding the challenges inherent in diagnosing Parkinson’s early, and the crucial role of lifestyle management, are also key components of this comprehensive overview.
Disease Mechanisms and Progression
Parkinson’s disease (PD) is a complex neurodegenerative disorder characterized by the progressive loss of dopaminergic neurons in the substantia nigra pars compacta of the brain. While the exact cause remains elusive, significant advancements have been made in understanding its pathogenesis and progression.
Alpha-Synuclein Aggregation in Parkinson’s Disease Pathogenesis
The current understanding of PD pathogenesis centers around the misfolding and aggregation of alpha-synuclein (α-syn), a protein normally found in presynaptic nerve terminals. These misfolded α-synuclein proteins aggregate to form Lewy bodies, intracellular inclusions that are a pathological hallmark of PD. The aggregation process is believed to trigger a cascade of events, including neuronal dysfunction, inflammation, and ultimately, cell death. The precise mechanisms by which α-synuclein aggregation leads to neurodegeneration are still under investigation, but several hypotheses involve oxidative stress, mitochondrial dysfunction, and impaired protein degradation pathways. The spread of α-synuclein aggregates from one neuron to another, a process termed “bradykinesia,” is also thought to contribute to the progressive nature of the disease.
Stages of Parkinson’s Disease Progression and Associated Symptoms
Parkinson’s disease progression is typically described in stages, although the rate of progression varies significantly between individuals. Early stages may involve subtle motor symptoms like tremor, rigidity, and bradykinesia (slowness of movement) affecting one side of the body. As the disease progresses, these symptoms become more pronounced and bilateral, impacting gait, balance, and coordination. Later stages are characterized by severe motor impairments, significant disability, and the emergence of non-motor symptoms such as cognitive decline, sleep disturbances, and depression. The Hoehn and Yahr scale is a commonly used clinical staging system, although it doesn’t capture the full spectrum of non-motor symptoms.
Genetic and Environmental Risk Factors in Parkinson’s Disease
Both genetic and environmental factors contribute to the risk of developing PD. A number of genes have been identified that increase susceptibility, including those involved in α-synuclein metabolism (SNCA), autophagy (LRRK2, GBA), and mitochondrial function (PINK1, PARKIN). However, most cases of PD are sporadic, meaning they don’t have a clear genetic cause. Environmental factors, such as exposure to pesticides, herbicides, and heavy metals, have also been linked to an increased risk of PD. The interplay between genetic predisposition and environmental exposures is likely crucial in determining an individual’s susceptibility. For example, individuals with a genetic predisposition might be more vulnerable to the neurotoxic effects of environmental toxins.
Neurobiological Changes During Parkinson’s Disease Progression
The neurobiological changes in PD are multifaceted and progressive. The most prominent feature is the loss of dopaminergic neurons in the substantia nigra, leading to dopamine deficiency in the striatum. This dopamine deficiency underlies the cardinal motor symptoms of PD. However, the disease also affects other brain regions and neurotransmitter systems, contributing to the wide range of motor and non-motor symptoms. Neuroinflammation, oxidative stress, and glial cell dysfunction also play significant roles in the disease process.
| Stage | Motor Symptoms | Non-Motor Symptoms | Neuropathological Hallmarks |
|---|---|---|---|
| Early | Tremor, rigidity, bradykinesia (one side) | Constipation, sleep disturbances, loss of smell | Mild dopamine neuron loss in substantia nigra, Lewy bodies |
| Moderate | Bilateral motor symptoms, gait instability | Cognitive impairment, depression, anxiety | More pronounced dopamine neuron loss, increased Lewy body burden |
| Advanced | Severe motor impairment, dependence on assistance | Significant cognitive decline, dementia, autonomic dysfunction | Extensive dopamine neuron loss, widespread Lewy body pathology |
Current Treatment Approaches
Parkinson’s disease, a progressive neurodegenerative disorder, currently lacks a cure. However, a range of treatments are available to manage symptoms and improve quality of life. These approaches encompass pharmacological interventions, surgical options, and non-pharmacological therapies, each with its own set of benefits and limitations. The optimal treatment strategy is highly individualized, depending on the severity of symptoms, the patient’s overall health, and personal preferences.
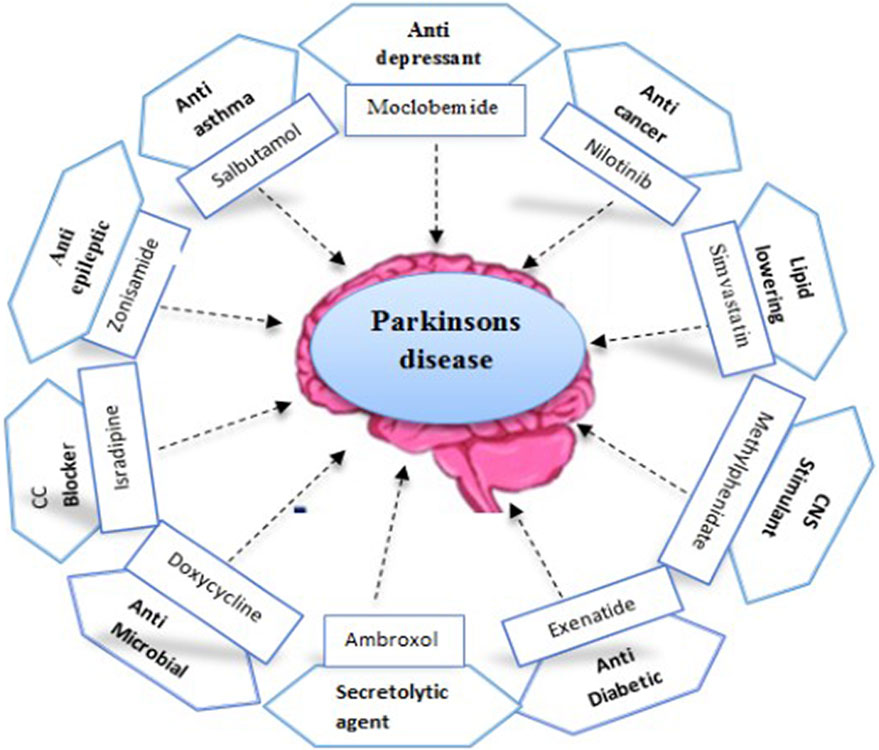
Pharmacological Treatments
Pharmacological management of Parkinson’s disease primarily focuses on replenishing dopamine levels in the brain or modulating the activity of dopamine pathways. Levodopa, a precursor to dopamine, remains the gold standard for treating motor symptoms. Dopamine agonists mimic the effects of dopamine, while MAO-B inhibitors prevent the breakdown of dopamine, thus increasing its availability. However, each of these medications comes with potential side effects that must be carefully considered.
Levodopa, while highly effective in improving motor function in the early stages of the disease, can lead to motor fluctuations (wearing-off and on-off phenomena) and dyskinesias (involuntary movements) with prolonged use. Dopamine agonists, while useful as monotherapy or in combination with levodopa, can also cause similar motor complications, along with potential side effects such as nausea, hallucinations, and sleep disturbances. MAO-B inhibitors offer a milder effect on motor symptoms and are often used as adjunctive therapy, particularly in the early stages of the disease, or to delay the need for levodopa. However, their effectiveness is generally less pronounced than levodopa or dopamine agonists.
Surgical Interventions: Deep Brain Stimulation (DBS)
Deep brain stimulation (DBS) is a surgical procedure that involves implanting electrodes into specific brain regions to modulate neuronal activity. This technique is primarily used for advanced Parkinson’s disease patients who experience significant motor fluctuations and dyskinesias unresponsive to medication. DBS can significantly improve motor symptoms, reduce medication requirements, and enhance quality of life for many patients. However, DBS is an invasive procedure with potential risks, including bleeding, infection, and equipment malfunction. Careful patient selection and pre-operative assessment are crucial to ensure the procedure’s success and minimize potential complications.
Non-Pharmacological Therapies
Non-pharmacological therapies play a vital role in managing Parkinson’s disease symptoms and improving overall well-being. These therapies address both motor and non-motor symptoms and are often used in conjunction with pharmacological interventions.
Physical therapy focuses on improving mobility, strength, balance, and coordination through exercises tailored to the individual’s needs and capabilities. Occupational therapy assists patients in adapting their daily activities and environment to maintain independence and function. Speech therapy helps individuals manage communication and swallowing difficulties. Other non-pharmacological approaches include cognitive behavioral therapy (for managing depression and anxiety), support groups, and lifestyle modifications (diet, exercise, and stress management).
Comparison of Treatment Strategies for Motor and Non-Motor Symptoms
The effectiveness of different treatment strategies varies depending on the specific symptom being addressed.
- Motor Symptoms: Levodopa remains the most effective medication for improving motor symptoms, especially in the early stages. However, long-term use can lead to motor complications. DBS can provide significant benefit in advanced cases refractory to medication. Physical therapy plays a crucial role in maintaining mobility and functional independence.
- Non-Motor Symptoms: Non-pharmacological approaches, such as cognitive behavioral therapy and support groups, are often the first line of treatment for non-motor symptoms like depression, anxiety, and sleep disturbances. Pharmacological interventions may be necessary in some cases, but their effectiveness can be limited and side effects can be significant.
Emerging Therapeutic Strategies
The search for effective treatments for Parkinson’s disease (PD) extends beyond current symptomatic therapies. Significant research efforts are focused on developing disease-modifying strategies that can slow or halt disease progression, ultimately improving the quality of life for individuals with PD. These emerging therapeutic strategies hold considerable promise and represent a significant shift in the approach to managing this debilitating condition.
Neuroprotection and Disease Modification
Neuroprotective strategies aim to prevent the death of dopamine-producing neurons in the substantia nigra, the brain region most affected in PD. Disease modification strategies go a step further, seeking to address the underlying mechanisms that cause the disease’s progression. This includes targeting alpha-synuclein aggregation, mitochondrial dysfunction, and neuroinflammation. Several promising avenues of research are being pursued, including the development of drugs that can enhance neuronal survival, reduce oxidative stress, and modulate immune responses within the brain. For example, research into the role of specific antioxidants and anti-inflammatory agents shows promise in preclinical models, suggesting potential future clinical applications.
Novel Therapeutic Agents Under Investigation
Several novel therapeutic agents are currently under investigation, employing diverse mechanisms of action. These include:
- Chaperone proteins: These proteins assist in the proper folding and degradation of proteins, potentially preventing the aggregation of alpha-synuclein, a hallmark of PD.
- Mitochondrial targeted therapies: These agents aim to improve mitochondrial function, which is often impaired in PD. Examples include compounds that enhance mitochondrial biogenesis or protect against mitochondrial damage.
- Anti-inflammatory agents: Chronic neuroinflammation contributes to neuronal damage in PD. Therefore, the development of anti-inflammatory drugs targeting specific inflammatory pathways holds promise for disease modification.
- Modulators of alpha-synuclein aggregation: Research focuses on identifying and developing compounds that can prevent or reverse the aggregation of alpha-synuclein, thereby slowing or halting the progression of the disease. Several molecules are currently in preclinical or early clinical trials showing some efficacy in reducing alpha-synuclein levels.
Gene Therapy and Cell-Based Therapies
Gene therapy approaches aim to introduce genetic material into cells to correct or compensate for genetic defects or to enhance the production of beneficial proteins. For PD, this might involve delivering genes that promote dopamine production or protect against neuronal damage. Early clinical trials have shown some encouraging results, though further research is needed to optimize delivery methods and ensure long-term safety and efficacy. Cell-based therapies, on the other hand, involve transplanting healthy cells into the brain to replace damaged dopamine-producing neurons. Stem cell transplantation is a promising approach, with ongoing clinical trials evaluating its potential to improve motor function and other symptoms.
Immunotherapy Targeting Alpha-Synuclein and Other Disease-Related Proteins
Immunotherapy aims to harness the power of the immune system to target and eliminate alpha-synuclein aggregates or other disease-related proteins. This can be achieved through active or passive immunization strategies. Active immunization involves stimulating the immune system to produce antibodies against alpha-synuclein, while passive immunization involves directly administering antibodies that can bind to and neutralize alpha-synuclein. Early clinical trials using active immunization have shown mixed results, highlighting the complexities of designing effective and safe immunotherapy strategies for neurodegenerative diseases. However, the ongoing research in this area continues to explore various approaches, including targeting different epitopes of alpha-synuclein and employing different antibody delivery methods.
| Emerging Therapeutic Strategy | Mechanism of Action | Current Stage of Development | Potential Benefits |
|---|---|---|---|
| Neuroprotective Agents | Prevent neuronal death, reduce oxidative stress | Preclinical and early clinical trials | Slow disease progression, preserve neuronal function |
| Gene Therapy | Introduce genes to enhance dopamine production or neuroprotection | Early clinical trials | Disease modification, potential for long-term benefits |
| Cell-Based Therapies (e.g., stem cell transplantation) | Replace damaged dopamine-producing neurons | Clinical trials | Improve motor function, reduce symptoms |
| Immunotherapy (targeting alpha-synuclein) | Eliminate alpha-synuclein aggregates through immune response | Early clinical trials | Reduce protein aggregation, slow disease progression |
Diagnostic Advancements
Diagnosing Parkinson’s disease (PD) currently relies on a combination of clinical evaluation and supportive diagnostic tests. While there’s no single definitive test, advancements in neuroimaging and biomarker research are steadily improving diagnostic accuracy and enabling earlier detection.
Current diagnostic methods primarily focus on identifying the characteristic motor symptoms of PD, such as tremor, rigidity, bradykinesia (slow movement), and postural instability. A detailed neurological examination, including assessment of these motor symptoms and their asymmetry, forms the cornerstone of diagnosis. However, this approach has limitations, as early-stage PD symptoms can be subtle and easily confused with other neurological conditions. Furthermore, the clinical presentation can vary significantly between individuals, leading to diagnostic challenges.
Neuroimaging Techniques in Parkinson’s Disease Diagnosis
Neuroimaging techniques play a crucial role in improving diagnostic accuracy by visualizing brain structures and function. Magnetic Resonance Imaging (MRI) is widely used to rule out other neurological conditions that mimic PD, such as stroke or brain tumors. Structural MRI can sometimes reveal subtle changes in brain regions affected by PD, though these changes are often not specific enough for definitive diagnosis. Positron Emission Tomography (PET) scans, using tracers that bind to dopamine transporters (DAT) or other neurochemicals, offer more specific information about dopaminergic function in the brain. Reduced DAT binding in the striatum, a brain region crucial for movement control, is a strong indicator of PD. However, PET scans are expensive and not always readily available. Furthermore, some individuals with PD may show normal DAT binding, particularly in early stages. Functional MRI (fMRI) can also contribute by assessing brain activity during motor tasks, potentially revealing patterns associated with PD.
Potential Biomarkers for Early Diagnosis and Disease Monitoring
Identifying reliable biomarkers in blood, cerebrospinal fluid (CSF), or other bodily fluids is a key area of ongoing research. These biomarkers could potentially allow for earlier diagnosis, even before the onset of motor symptoms, and facilitate monitoring of disease progression and response to treatment. Several potential biomarkers are currently under investigation, including alpha-synuclein, a protein that aggregates in the brains of individuals with PD, and various inflammatory markers. However, consistent and reliable detection of these biomarkers in easily accessible samples remains a challenge. Further research is needed to validate these potential biomarkers and develop standardized assays for their detection.
Novel Diagnostic Tools for Improved Accuracy and Speed
Researchers are actively developing novel diagnostic tools to improve the accuracy and speed of PD diagnosis. These include advanced neuroimaging techniques, such as advanced MRI sequences providing higher resolution and more sensitive measures of brain structure and function, and more sophisticated analysis of PET scan data using machine learning algorithms. Furthermore, research into easily accessible biomarkers, like those found in saliva or blood, continues to progress, with the potential to provide a simple and cost-effective screening tool. Development of digital biomarkers, analyzing subtle changes in gait, speech, or handwriting through wearable sensors and smartphone apps, shows promise for early detection and remote monitoring.
Summary of Diagnostic Advancements
| Method | Description | Strengths | Weaknesses |
|---|---|---|---|
| Clinical Examination | Assessment of motor symptoms | Relatively inexpensive and widely available | Subjective, relies on symptom presentation, can be inaccurate in early stages |
| MRI | Imaging of brain structure | Can rule out other conditions | Often non-specific for PD |
| DAT-SPECT/PET | Imaging of dopamine transporters | High specificity for PD | Expensive, not widely available, may be normal in early stages |
| Biomarker Analysis | Detection of molecules in blood/CSF | Potential for early diagnosis and disease monitoring | Lack of validated and reliable biomarkers |
Lifestyle Factors and Disease Management
Parkinson’s disease, while a progressive neurological condition, is not solely determined by genetics. Lifestyle significantly influences disease progression and overall quality of life for individuals affected. Understanding and implementing positive lifestyle changes can contribute meaningfully to managing symptoms and improving well-being. This section will explore the crucial role of lifestyle factors, supportive care, and addressing non-motor symptoms in a comprehensive Parkinson’s disease management plan.
Diet’s Impact on Parkinson’s Disease Progression
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins is recommended for individuals with Parkinson’s disease. Research suggests that certain dietary patterns, such as the Mediterranean diet, may offer neuroprotective benefits. Conversely, diets high in saturated and trans fats may exacerbate inflammation and potentially accelerate disease progression. Specific nutrients, like antioxidants found in berries and leafy greens, are believed to combat oxidative stress, a key factor in Parkinson’s pathogenesis. Furthermore, maintaining a healthy weight is crucial, as obesity is associated with increased risk and severity of motor symptoms. Regular monitoring of dietary intake and consultation with a registered dietitian can help individuals tailor their nutrition to their specific needs and preferences.
Exercise and Physical Activity in Parkinson’s Disease
Regular physical activity plays a vital role in managing Parkinson’s disease symptoms. Exercise programs, tailored to individual capabilities, can improve motor skills, balance, and coordination. Aerobic exercises, such as walking, swimming, or cycling, enhance cardiovascular health and may also have neuroprotective effects. Strength training helps maintain muscle mass and strength, mitigating the impact of muscle weakness often associated with the disease. Flexibility and balance exercises are equally important in preventing falls and improving overall mobility. A structured exercise program, ideally under the guidance of a physical therapist experienced in working with Parkinson’s patients, is highly recommended.
Sleep Hygiene and its Significance
Sleep disturbances, including insomnia, REM sleep behavior disorder, and excessive daytime sleepiness, are common non-motor symptoms in Parkinson’s disease. These sleep problems can significantly impact quality of life, exacerbating motor symptoms and cognitive impairment. Establishing good sleep hygiene practices, such as maintaining a regular sleep schedule, creating a relaxing bedtime routine, and optimizing the sleep environment, is crucial. Cognitive behavioral therapy for insomnia (CBT-I) can be particularly effective in addressing insomnia. Furthermore, clinicians should carefully evaluate and address any underlying sleep disorders to improve sleep quality and overall well-being.
Supportive Care and Patient Education
Supportive care extends beyond medical treatments and encompasses various strategies to enhance the overall well-being of individuals with Parkinson’s disease. Patient education is paramount, empowering individuals and their caregivers with knowledge about the disease, its management, and available resources. This includes understanding medication regimens, recognizing symptom fluctuations, and proactively addressing potential complications. Support groups provide a platform for sharing experiences, coping strategies, and emotional support. Occupational therapy can help adapt daily tasks to accommodate physical limitations, maintaining independence and improving quality of life. Speech therapy may be beneficial for individuals experiencing communication difficulties.
Addressing Non-Motor Symptoms
Non-motor symptoms, such as depression, anxiety, cognitive impairment, and constipation, significantly impact the quality of life for individuals with Parkinson’s disease. These symptoms often precede or accompany motor symptoms and require specific management strategies. Depression and anxiety can be effectively treated with medication, therapy, or a combination of both. Cognitive impairment may necessitate cognitive rehabilitation strategies or medication to enhance cognitive function. Addressing constipation often involves dietary modifications and, if necessary, medication. Regular monitoring and proactive management of these non-motor symptoms are crucial components of a holistic approach to Parkinson’s disease management.
Comprehensive Management Plan Recommendations
A comprehensive management plan for Parkinson’s disease should incorporate the following:
- Regular visits with a neurologist specializing in movement disorders.
- A personalized medication regimen to manage motor and non-motor symptoms.
- A structured exercise program, including aerobic exercise, strength training, and balance exercises.
- Dietary modifications emphasizing a balanced diet rich in fruits, vegetables, and whole grains.
- Prioritization of sleep hygiene practices to improve sleep quality.
- Participation in support groups and access to patient education resources.
- Proactive management of non-motor symptoms, such as depression, anxiety, and cognitive impairment.
- Regular monitoring of disease progression and adjustment of treatment strategies as needed.
Challenges and Future Directions
Despite significant advancements in understanding Parkinson’s disease (PD), substantial challenges remain in developing effective treatments. The lack of disease-modifying therapies that can slow or halt the progression of the disease is a major hurdle. Current treatments primarily focus on managing symptoms, offering only limited impact on the underlying neurodegenerative process. This necessitates a continued and intensified research effort to overcome these obstacles and improve the lives of those affected by PD.
The need for a deeper understanding of the complex mechanisms driving PD progression is paramount. While the loss of dopaminergic neurons in the substantia nigra is a hallmark of the disease, the precise sequence of events leading to this neuronal degeneration and the contribution of various genetic and environmental factors remain incompletely understood. This knowledge gap hinders the development of truly effective disease-modifying therapies. Furthermore, the heterogeneity of PD, with varying symptom profiles and disease trajectories among individuals, adds complexity to research and treatment development.
Understanding Disease Mechanisms and Identifying Novel Therapeutic Targets
A critical challenge lies in fully elucidating the complex interplay of genetic, environmental, and epigenetic factors contributing to PD pathogenesis. While several genes have been linked to increased risk, their precise roles and interactions remain unclear. Similarly, the impact of environmental toxins, such as pesticides and heavy metals, on PD risk requires further investigation. Unraveling these intricate relationships is crucial for identifying novel therapeutic targets and developing personalized medicine approaches tailored to individual patient profiles. For example, research into α-synuclein aggregation, a key pathological feature of PD, continues to be a major focus, aiming to develop therapies that can prevent or reverse this process. Another area of intense investigation is the role of neuroinflammation and its potential as a therapeutic target.
Collaborative Research and Multidisciplinary Approaches
Progress in PD research necessitates a collaborative, multidisciplinary approach, bringing together expertise from various fields including neuroscience, genetics, pharmacology, bioengineering, and clinical neurology. Large-scale, international collaborations are essential for conducting robust clinical trials and sharing data efficiently. For instance, the Michael J. Fox Foundation has played a significant role in fostering such collaborations, facilitating the sharing of research data and accelerating the development of new therapies. These collaborative efforts are crucial for addressing the complexity of PD and overcoming the limitations of single-investigator studies.
Future Directions and Potential Breakthroughs
The future of PD research holds considerable promise. Advances in gene editing technologies, such as CRISPR-Cas9, offer the potential for developing gene therapies that can correct genetic defects associated with PD. Furthermore, the development of novel biomarkers, capable of detecting the disease in its early stages, will allow for earlier intervention and potentially slow or prevent disease progression. Advances in stem cell therapy and brain stimulation techniques also hold considerable promise for improving treatment outcomes. While significant challenges remain, the ongoing research efforts across the globe offer hope for breakthroughs in the prevention and treatment of Parkinson’s disease. The development of disease-modifying therapies remains a primary goal, with several promising candidates currently undergoing clinical trials. Success in this area would represent a paradigm shift in the management of PD, transforming it from a progressive, debilitating condition to one that can be effectively managed or even prevented.
Last Point
In conclusion, the landscape of Parkinson’s disease research is dynamic and brimming with potential. While significant challenges remain, particularly the lack of disease-modifying therapies, ongoing advancements in our understanding of disease mechanisms and the development of innovative treatments offer considerable hope. A collaborative, multidisciplinary approach, integrating research, clinical practice, and patient advocacy, is crucial to accelerating progress and ultimately improving the lives of those affected by this devastating illness. The future of Parkinson’s treatment is promising, with ongoing research paving the way for more effective interventions and a better quality of life for patients.